Face Reconstruction with Microsurgical and Craniofacial Techniques
Gesichtsrekonstruktion mit mikrochirurgischen und craniofacialen Techniken
Lars H. Evers
1,2,3Fu-Chan Wei
2Eric Arnaud
3Uwe von Fritschen
11 Department of Plastic Surgery, Behring Hospital, Academic Hospital of Charite University Medicine, Berlin, Germany
2 Division of Microsurgery, Department of Plastic and Reconstructive Surgery, Chang Gung Memorial Hospital, Taipei, Taiwan 3 National Reference Center
for Craniofacial Surgery, Hospital Necker Enfants Malades, Paris, France
Background
Large, composite defects in the craniofacial region are still an enormous reconstructive challenge. The fusion of soft and hard tissue especially in the face as a delicate anatomical region requires a multitude of different tech- niques and refinements. Deficiencies of both the facial skeleton and the overlying soft tissue must be addressed to achieve the optimal reconstructive functional and aesthetic result. Several novel techniques evolved over the past decades based on advances in craniofacial and microsurgery. These two disciplines begun to overlap more frequently, and the techniques of one have been used to advance the other. In the current study, the au- thors present their personal experiences and aim to de- scribe the available options for free tissue transfer to the face as well as highly advanced craniofacial techniques to correct congenital, posttraumatic and oncologic de- fects.
Methods
Here we present our combined institutional experience with 85 patients over a period of 2 years who underwent facial reconstruction including microsurgical soft and hard tissue reconstructions as well as complex craniofa- cial reconstructions. The follow-up was at least 6 months.
Furthermore a review of microsurgical and craniofacial reconstructive options of aesthetic units within the craniofacial region was undertaken with attention directed toward surgeon preference.
Results
The anatomical areas analyzed included scalp, calvaria, forehead, frontal sinus, nose, maxilla and midface, peri- orbita, mandible, lip, and tongue. Although certain flaps such as the anterolateral thigh flap (ALT) were used in multiple reconstructive sites, each anatomical location possesses a unique array of flaps to maximize outcomes.
The overall free flap survival rate was 98.4%. Major
1/3 GMS German Plastic, Reconstructive and Aesthetic Surgery 2016, Vol. 6, ISSN 2193-7052
Extended Abstract
OPEN ACCESS
Best Abstract Award DGPRÄC 2015
Figure 1: a) 61-year-old gentleman with a left buccal squamous cell cancer with a history of betel nut chewing over several years. The intra-operative view shows the large soft and hard tissue defect after the oncologic resection. b) Early post-operative view after defect coverage with a double free flap (free fibula flap to restore the mandible defect and free ALT flap to cover the
soft tissue deficit).
Table 1: Results from complex face reconstructions using microsurgical techniques. Please note, that in some cases several free flaps per patient were performed.
complications (revisions, major hematoma, infections) occurred in 9.5%, minor complications (wound dehiscence etc.) occurred in 12.7%. The underlying defects included oncologic cases (Figure 1), posttraumatic defects as well as congenital deformities. Some of the patients had pre- vious facial skeletal correction using craniofacial tech- niques. The age at operation ranged from 3 to 78 years.
The most common applied flaps were anterolateral thigh flap (ALT), free fibula flap +/- skin paddle and in some cases with soleus muscle as an osteomyocutaneous peroneal artery-based composite (OPAC) flap. Furthermore we used parascapular flaps, radial and ulnar forearm flaps, sural artery perforator flaps and gracilis muscle free flaps (Table 1).
Conclusions
Craniofacial surgery, like plastic surgery, has made tre- mendous advancements in the past decades. With innov- ations in technology, flap design, and training, microsur- gery has become safer, faster, and more common than in previous decades. Reconstructive microsurgery allows the surgeon to be creative in his approach, and free tissue transfer has become a mainstay of modern craniofacial reconstruction. Correction of facial contour in complex
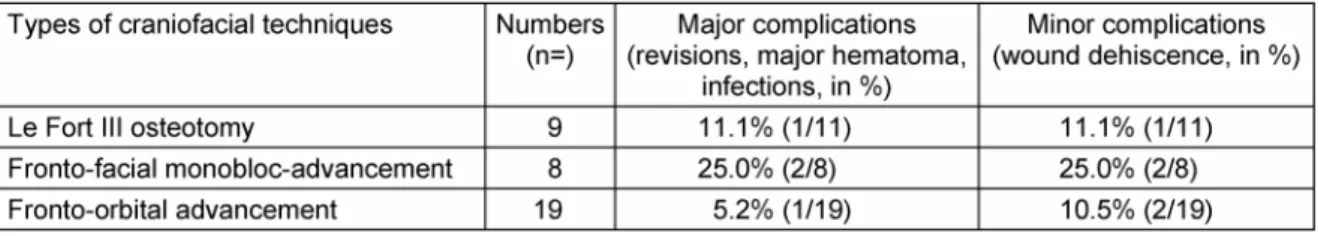
craniofacial defects is possible using microsurgical tech- niques. These free flaps “camouflage” the underlying skeletal deformity that persists sometimes despite tradi- tional skeletal reconstruction while restoring symmetrical facial contour. Our results show, that the overall free flap survival rate in these challenging reconstructive cases can be very high. The ALT as a workhorse free flap is in our hands a versatile and reliable flap and shows a low complication rate. The results in the complex facial recon- structions using craniofacial techniques also show a high success rate due to the extraordinary expertise of this reference center. The fronto-facial Monobloc Advance- ment is a very effective procedure, however it shows a higher complication rate than other traditional craniofacial techniques (Table 2). We recommend the “marriage” of both skeletal and microsurgical soft-tissue reconstructions to achieve the optimal functional and aesthetic result for craniofacial contouring in these challenging patients.
2/3 GMS German Plastic, Reconstructive and Aesthetic Surgery 2016, Vol. 6, ISSN 2193-7052
Evers et al.: Face Reconstruction with Microsurgical and Craniofacial ...
Table 2: Results from complex face reconstructions using craniofacial techniques. Please note, that in some cases several techniques per patient were performed.
Competing interests
The authors declare that they have no competing in- terests.
Note
At the 46thmeeting of the German Society of Plastic, Re- constructive and Aesthetic Surgeons (DGPRÄC) the cor- responding abstract [1] was awarded “Best Abstract”.
The society highlighted the best abstract submissions with this award in 2015. The publication of the extended abstract in GMS German Plastic, Reconstructive and Aesthetic Surgery – Burn and Hand Surgery was sponsored by “Amryt Pharma”.
References
1. Evers LH, Wei FC, Arnaud E, von Fritschen U. Face reconstruction with microsurgical and craniofacial techniques. In: 46.
Jahrestagung der Deutschen Gesellschaft der Plastischen, Rekonstruktiven und Ästhetischen Chirurgen (DGPRÄC), 20.
Jahrestagung der Vereinigung der Deutschen Ästhetisch- Plastischen Chirurgen (VDÄPC); 2015 Oct 1-3; Berlin. Düsseldorf:
German Medical Science GMS Publishing House; 2015. Doc203.
DOI: 10.3205/15dgpraec203
Corresponding author:
Lars H. Evers
Department of Plastic Surgery, Behring Hospital, Academic Hospital of Charite University Medicine, Walterhöferstr. 11, 14165 Berlin, Germany Lars.Evers@helios-kliniken.de
Please cite as
Evers LH, Wei FC, Arnaud E, von Fritschen U. Face Reconstruction with Microsurgical and Craniofacial Techniques. GMS Ger Plast Reconstr Aesthet Surg. 2016;6:Doc06.
DOI: 10.3205/gpras000041, URN: urn:nbn:de:0183-gpras0000419
This article is freely available from
http://www.egms.de/en/journals/gpras/2016-6/gpras000041.shtml Published:2016-09-29
Copyright
©2016 Evers et al. This is an Open Access article distributed under the terms of the Creative Commons Attribution 4.0 License. See license information at http://creativecommons.org/licenses/by/4.0/.
3/3 GMS German Plastic, Reconstructive and Aesthetic Surgery 2016, Vol. 6, ISSN 2193-7052
Evers et al.: Face Reconstruction with Microsurgical and Craniofacial ...