AUS DEM LEHRSTUHL FÜR ORTHOPÄDIE DIREKTOR PROF. DR. MED. DR. H.C. J. GRIFKA DER FAKULTÄT FÜR MEDIZIN DER UNIVERSITÄT REGENSBURG
Volltext
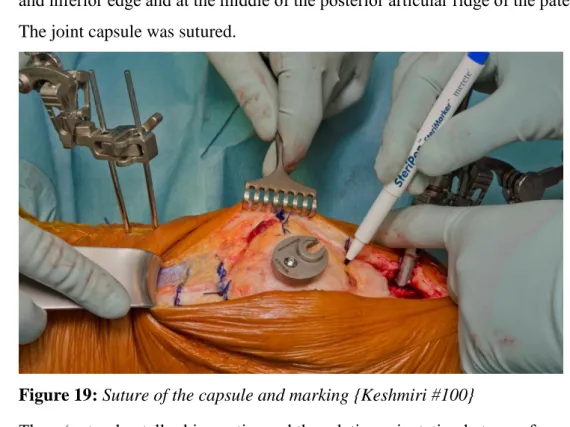
Abbildung
ÄHNLICHE DOKUMENTE
Zusammenfassend kann man sagen, dass sich in unserer Studie sowohl deutliche Vorteile für die Patienten nach erfolgreicher Pankreastransplantation im Vergleich zur Einstellung
Die Verschiebung in der Altersstruktur als Folge von niedrigen Geburtenraten und steigender Lebenserwartung ist ein Phänomen, welches die Bundesrepublik Deutschland vor neue
Da sich IL-6 nach einer Endoprothesenimplantation innerhalb von 2 Tagen normalisiert, kann dies ein sensitiver Indikator für eine periprothetische Infektion in der
Auch in der Indikation der rheumatoiden Arthritis fallen Unterschiede in den jeweiligen Fachinformationen auf. Zunächst zeigen sich
Diese Kenntnisse über das implizite Gedächtnis legen die Vermutung nahe, dass sich Patienten nach der Implantation einer Knieendoprothese unter Sedierung zwar
In mehreren Studien konnte nachgewiesen werden, dass die katabolischen Effekte auf den Knorpel unter anderem über eine Hemmung der die Chondrogenese fördernden Faktoren TGF-ß
Diese Druckerhöhung wird unter anderem dadurch erklärt, dass es bei den Patienten im Bereich des Hüftkopfes zu einer venösen Stase kommt, da nicht nur die Anzahl
Dabei verwendet man T1 gewichtete Bilder, um Ausdehnung, Gruppierung und Homogenität der Läsion zu beurteilen, T2 gewichtete Darstellungen, um den Knorpel und die